If you have spent more than twelve minutes in a pair of scrubs, you’ve heard the term “The Nursing Shortage” whispered in the hallways like a ghost story told around a flickering breakroom microwave. It’s presented to the public as this mysterious, unavoidable phenomenon—like a drought or a bad crop of kale.
But let’s be real: we aren’t dealing with a shortage of nurses. If you threw a rock into a Target on a Tuesday morning, you’d probably hit three women in athletic wear who have an active RN license but chose to leave the bedside because they’d rather fold yoga pants than spend another twelve hours wondering if they’re going to lose their license because they were assigned six ICU-level patients on a Med-Surg floor.
The truth? We don’t have a shortage of nurses. We have a shortage of nurses who are willing to be treated like an Olympic sprinter expected to run a marathon while carrying two toddlers and a tray of lukewarm apple juice.
The Calculus of Chaos
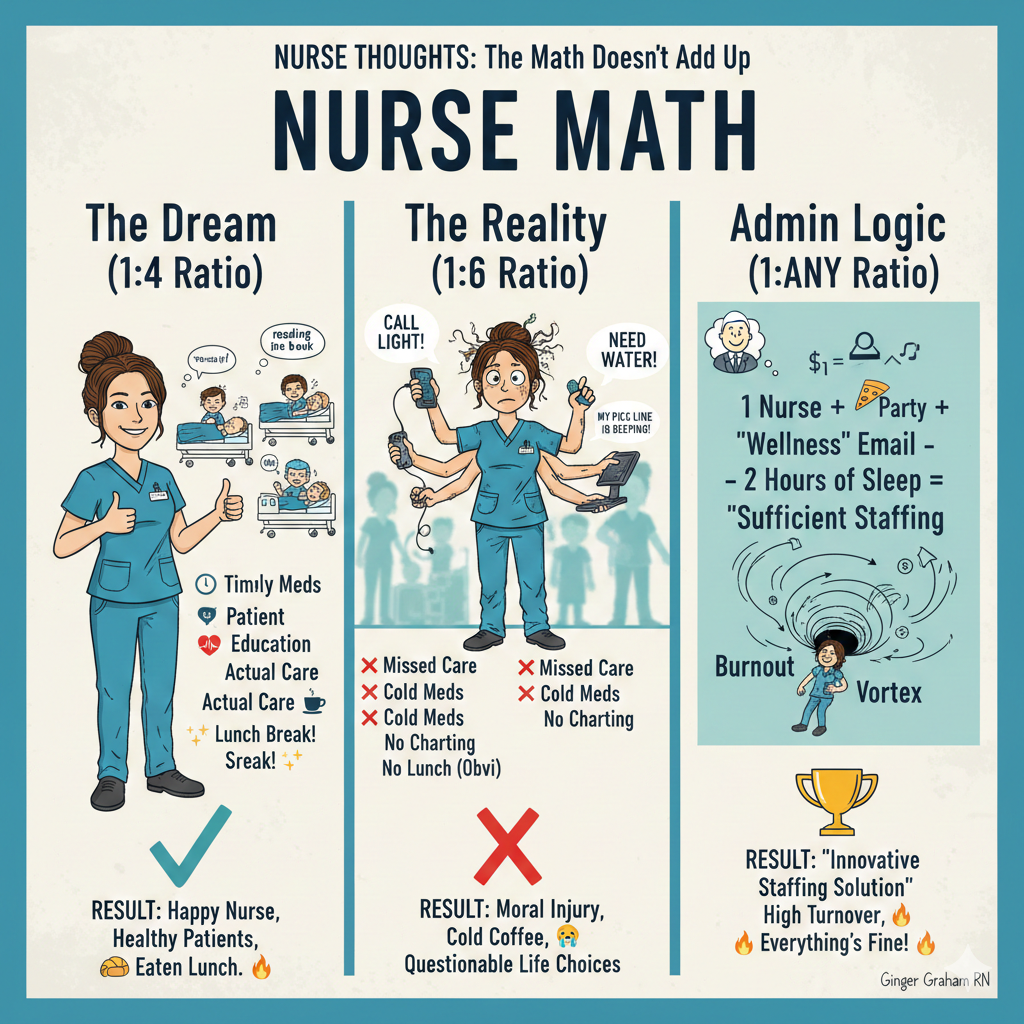
Let’s talk about the math. In the world of hospital administration, a nurse-to-patient ratio is often seen as a flexible suggestion—kind of like the “serving size” on a bag of Flamin’ Hot Cheetos. But for the nurse on the floor, the difference between a 1:4 and a 1:6 ratio isn’t just two more people. It is a fundamental shift in the space-time continuum.
When you have four patients, you can almost—almost—be the nurse you imagined you’d be when you were in nursing school, starry-eyed and holding a pristine stethoscope. You can actually listen to a lung sound for more than three seconds. You can explain to Mr. Johnson why he’s taking a blood thinner without looking at the door like a getaway driver during a bank heist.
But the moment that fifth or sixth patient is added to your board? You aren’t “providing care” anymore. you are “mitigating disasters.” You are triage-ing your own soul. You’re playing a high-stakes game of Tetris where the blocks are IV pumps, call lights, and the family member in Room 402 who wants to know why the ice chips aren’t “crunchy enough.”
As noted by the American Nurses Association (ANA), “appropriate nurse staffing is a critical clinical intervention.” It’s not a logistical preference; it is literally a form of treatment. When you thin that treatment out, the patient suffers. It’s like trying to make a gallon of soup with one single bouillon cube. Sure, it looks like soup, but nobody’s getting nourished.
The Nursing “Moral Injury” of the 1:6
We need to stop calling it “burnout.” Burnout implies that we just didn’t do enough yoga or forgot to drink our green juice. What we are actually experiencing is moral injury.
Moral injury happens when you know exactly what your patient needs—you know they need that dressing changed, you know they need to be turned to prevent a pressure ulcer, you know they need a compassionate ear because they just got a terminal diagnosis—but you physically cannot get to them because your other five patients are also in some version of crisis.
According to a landmark study published in The Lancet, researchers found that for every one-patient increase in a nurse’s workload, the likelihood of an inpatient dying within 30 days of admission increased by 7%. Read that again. It’s not just “stressful” for us; it’s lethal for them.
When I’m at a 1:6 ratio, I’m not a healthcare professional; I’m a professional juggler who is slowly realizing that three of the balls are actually live grenades. You spend your entire drive home in a “shift fog,” gripping the steering wheel and wondering, Did I actually document that output? Did I remember to tell the next shift that the lady in 210 has a weird allergy to latex? Did I eat today? (The answer to the last one is usually no, unless you count the half-chewed graham cracker you found in your pocket).
The Great Nursing Pivot: Where Did Everyone Go?
Hospital executives love to ask, “Where have all the nurses gone?” while staring at a breakroom that hasn’t seen a functional coffee maker since 2019.
They’ve gone to aesthetics. They’ve gone to remote case management. They’ve gone to school nursing where, yes, they deal with 400 kids, but at least nobody is crashing on a pressor while they’re trying to hand out a Band-Aid.
Nurses are pivoting because we are tired of being told that the solution to a systemic staffing crisis is a “Wellness Wednesday” email and a lukewarm pizza party. You cannot fix a 1:6 ratio with a pepperoni slice. It’s like trying to put out a forest fire with a Squirtle-themed water gun.
The National Council of State Boards of Nursing (NCSBN) has highlighted that the workload is the primary driver for nurses leaving the bedside within the first two years of practice. We are educating them, training them, and then throwing them into a woodchipper of “productivity metrics.”
The Solution: It’s Not Rocket Science (It’s Ratios)
So, how do we fix it? We look at the data.
California has had mandated nurse-to-patient ratios for two decades. Guess what? Their nurses stay longer, their patients die less, and—here’s the kicker for the bean counters—the hospitals actually save money.
When you have enough nurses, you have fewer falls. You have fewer hospital-acquired infections. You have shorter lengths of stay. You don’t have to pay a “travel nurse” $150 an hour to fill a gap because your staff nurses actually like their jobs enough to stay.
As the National Academy of Medicine emphasizes in their reports on the future of nursing, creating a healthy work environment is non-negotiable for the sustainability of the US healthcare system. This includes enforceable, acuity-based staffing.
“Acuity-based” is the key. Because let’s be honest, a 1:4 ratio of stable post-ops is a dream. A 1:4 ratio of four patients with “total care” needs, confused minds, and crashing blood pressures is a nightmare. We need staffing that looks at the person, not just the room number.
The Bottom Line in Nursing
If we want to “cure” the nursing shortage, we have to make the bedside a place where a sane person would want to work. We have to stop treating nurses like an infinite resource that can be stretched until they snap.
Until we get real about ratios, we’re just rearranging deck chairs on the Titanic. And frankly, I’m tired of the icebergs. I want to be the nurse I trained to be. I want to look my patients in the eye and know that I gave them 100%, not just the 16.6% I had left over after the administrative chaos.
So, the next time someone tells you there’s a nursing shortage, tell them the math doesn’t add up. We’re here. We’re ready. We just want to be able to do our jobs without losing our minds (or our licenses) in the process.
(Read More from Nurse Thoughts
- The Art of the 5-Minute Lunch: A Survival Guide (coming soon)
- Why Your ‘Nurse Brain’ Never Truly Turns Off (coming soon)
- 5 Things You Should Never Say to a Nurse on Hour 11 (coming soon)
- From Bedside to Blog: Why I Started Nurse Thoughts (coming soon)
- The Ultimate Guide to Compression Socks That Actually Stay Up (coming soon)
About the Author
Ginger Graham is the creator of Culinary Passages and Nurse Thoughts. With over a decade of experience in the healthcare trenches, Ginger has seen it all—from the chaos of the ER to the intricate dance of luxury travel planning. When she isn’t advocating for better staffing ratios or debunking healthcare myths, you can find her at Disneyland with her husband Brad and their two daughters, or at home trying to convince her Goldendoodle, Barnaby, that he is not, in fact, a lap dog. She believes in “no-fluff” reviews, clinical excellence, and that a good pair of leggings should never be see-through.