In nursing, the shift change report is more than a routine—it’s a lifeline. Every handoff is a critical moment where patient safety, continuity of care, and nursing communication come together. A smooth report allows the incoming nurse to start confidently, while a poorly structured one risks errors that could compromise care.
Think of it as a relay race: the baton must be passed smoothly for the team to succeed. A clear, concise, and professional nursing handoff ensures patients stay safe and teams function effectively.
This comprehensive guide will cover:
Why a strong shift report matters
Nurse handoff styles (including SBAR and bedside handoff)
Step-by-step instructions for effective communication
Pro tips, mnemonics, and tools to stay organized
Common mistakes to avoid
A sample SBAR script for real-world use
By the end, you’ll have everything you need to deliver stress-free, structured, and professional shift reports.
Why a Strong Shift Change Report Matters
1. Patient Safety
Research shows incomplete handoffs are among the leading causes of medical errors. A structured, detailed, but concise nurse handoff ensures vital information—like medication changes, test results, or new risks—doesn’t slip through the cracks.
2. Time Management
Organized reports prevent repetitive follow-up questions and wasted time. Instead of scrambling for details, incoming nurses can immediately focus on patient care.
3. Nurse Professionalism
Professional communication is the backbone of nursing. A well-delivered report demonstrates respect, competence, and accountability, setting a high standard for the unit.
4. Confidence & Trust
Leaving a shift knowing your patients are in good hands fosters team trust and personal confidence. Likewise, incoming nurses appreciate clear guidance that empowers them to succeed.
Keywords: shift report importance, patient safety in nursing, nurse professionalism, effective nurse handoff
Common Nurse Shift Report Styles
1. Traditional Verbal Report
Delivered face-to-face at the nurse’s station or bedside, this style builds rapport and allows clarification.
2. SBAR Nurse Report (Situation, Background, Assessment, Recommendation)
The SBAR format is one of the most effective and widely used. It structures information logically, making it easy to grasp quickly in busy environments.
3. Written or Electronic Report
Typically documented in electronic medical records (EMRs), this style provides consistency and documentation. However, it should be paired with a brief verbal handoff for context.
4. Bedside Handoff
Done in front of the patient, this encourages transparency and patient engagement. Nurses must remain mindful of HIPAA compliance during this process.
Keywords: SBAR nurse report, bedside handoff, EMR nurse report, nurse report styles
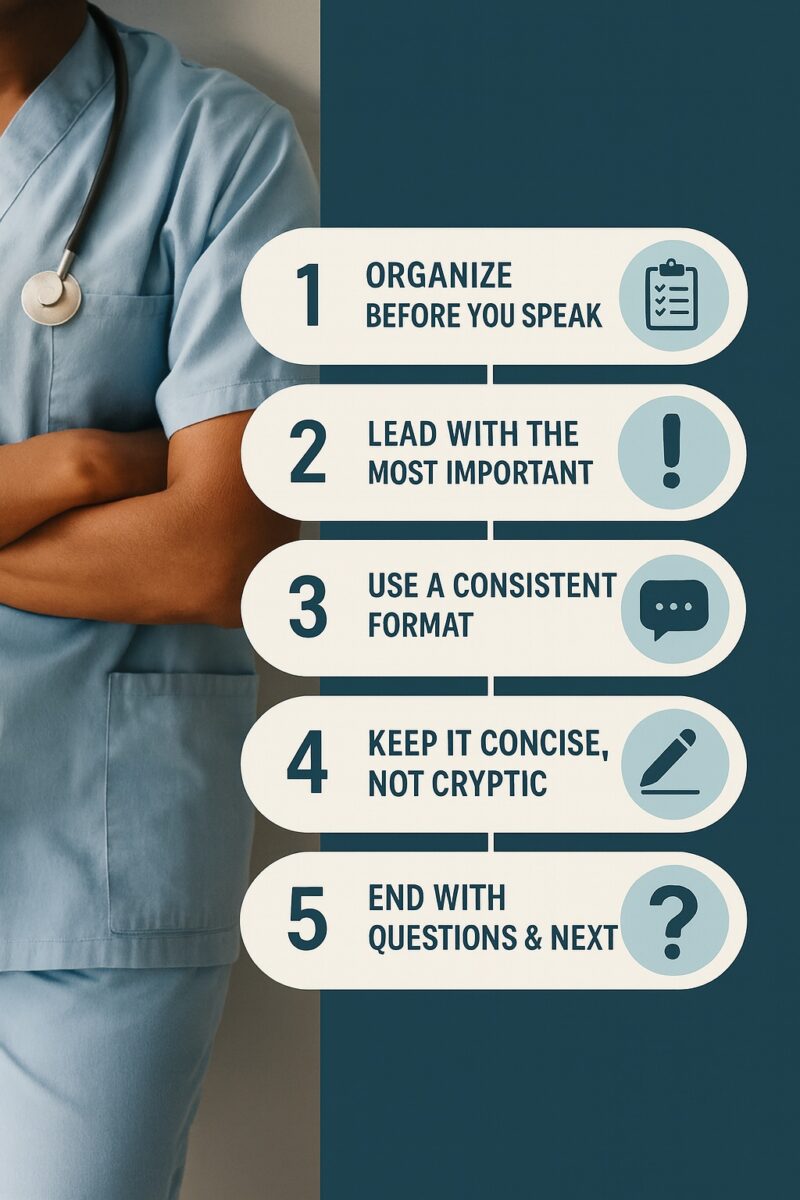
Step-by-Step: How to Give a Great Nurse Handoff
1. Organize Before You Speak
Preparation is key. Review vitals, labs, new orders, and your nurse brain sheet before handoff. Jot down any updates so nothing slips your memory.
2. Start with Critical Updates
Lead with urgent information. For example:
“Patient in Room 402 increased from 2L to 4L O₂ overnight due to desaturation. Currently stable, but still trending lower.”
3. Use a Consistent Format
Stick to SBAR or head-to-toe reports so your colleagues know exactly what to expect. Consistency prevents gaps.
4. Keep It Concise, Not Cryptic
Don’t overwhelm with unnecessary data. Share the relevant details for the next 12 hours of care. Clarity always beats complexity.
5. End with Engagement
Always conclude with:
“Any questions?”
“Things to watch for…”
This invites dialogue and ensures both sides are confident moving forward.
Pro Tips from Experienced Nurses
The “Top 3 Rule”: Always highlight the three most important concerns per patient.
Pending Tests: Share labs, imaging, or procedures waiting on results.
Red Zone Alerts: Point out critical risks like IV infiltrations, fall risk, or infection concerns.
Summarize Trends: Instead of saying “labs normal,” say: “Labs stable, slightly improved from yesterday.”
Use Mnemonics: Tools like SBAR, I-PASS (Illness severity, Patient summary, Action list, Situation awareness, Synthesis), or CUBAN (Condition, Urgency, Background, Action, Next) help retain structure.
Common Nurse Report Mistakes to Avoid
Information Dumping: Reading the chart verbatim overwhelms and confuses.
Personal Opinions: Stick to clinical facts. Subjectivity can skew decision-making.
Side Conversations: Distracts from patient safety. Stay focused.
HIPAA Violations: Never discuss patient information in public spaces like hallways or elevators.
Sample SBAR Nurse Handoff Script
Here’s a realistic example of how to structure your report:
S (Situation): “Room 312: 78-year-old female admitted with pneumonia. Stable on 3L O₂ via nasal cannula.”
B (Background): “History of COPD and diabetes. Admitted two days ago for increasing shortness of breath.”
A (Assessment): “Crackles in lungs, mild tachypnea overnight. Vitals otherwise stable. IV antibiotics infusing.”
R (Recommendation): “Monitor O₂ saturation closely, encourage incentive spirometer, next antibiotic due at 10:00.”
Tools & Templates for Better Handoffs
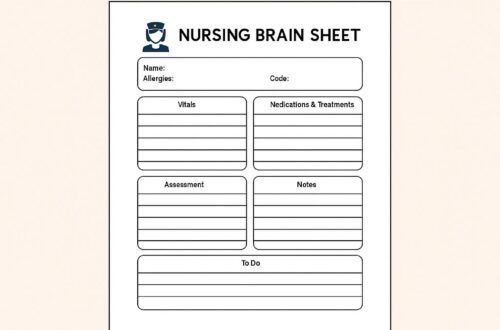
1. Nurse Brain Sheets
Printable nurse brain sheet templates help organize shift information and ensure nothing gets missed.
2. SBAR Cards
Small, pocket-sized SBAR reference cards act as quick guides for new nurses and students.
3. Mobile Apps & EMR Tools
Many hospitals now use secure apps integrated into EMRs to streamline reporting, improving consistency and compliance.
FAQs About Nursing Shift Change Reports
Q1: How long should a nurse handoff report take?
A good shift report should take 2–5 minutes per patient. Anything longer risks information overload.
Q2: What’s the best format for new nurses?
SBAR is highly recommended—it’s structured, concise, and easy to learn.
Q3: What should never be included in a shift report?
Personal opinions, irrelevant history, or non-care-related details. Stick to clinical facts.
Q4: Is bedside reporting better than traditional handoff?
Bedside handoff encourages patient engagement and accountability but requires HIPAA mindfulness. Many units use a hybrid approach.
Q5: How can nurse leaders improve handoffs on their units?
By implementing standardized formats (SBAR), training new staff, and providing templates for consistent, safe reporting.
Keywords: nurse handoff FAQs, effective nurse report, nursing communication best practices
Final Thoughts
Mastering the nurse shift change report is one of the most valuable skills for any RN. A well-structured handoff reduces errors, strengthens teamwork, builds professional credibility, and most importantly—keeps patients safe.
By using tools like SBAR nurse reports, brain sheets, and bedside handoff strategies, nurses can deliver efficient, stress-free reports every time. Avoiding common mistakes, staying consistent, and inviting questions ensures smooth transitions that empower both outgoing and incoming nurses.
Remember: every handoff is a chance to protect your patients and support your team.